The brain of any living organism, in general, is composed of millions of tiny cells called neurons. A human brain has over a billion neurons.
From cognitive tasks like reasoning, decision-making, and calculating to stimuli-based sensory responses to smells, touch or audio tracks – they all are linked to the neuronal wirings and inter-neuronal electrical pulse firings inside the brain occurring within microseconds.
Recently, a team of neuroscientists at the National Centre for Biological Sciences (NCBS), Bengaluru, has discovered a spike in a certain lipid in the brain linked to breakdown of this smooth neuronal communication in patients diagnosed with Lowe Syndrome (LS), a rare genetic disorder. And the team could possibly have answers to treat or design therapies for patients suffering from this rare genetic disorder simultaneously affecting the brain, eyes and kidney.
LS is a rare genetic disorder that affects one in 5,00,000, globally. In India, the prevalence of LS remains to be determined.
“We wanted to understand how people with LS suffer from multi-organ dysfunctions. Importantly, it strikes at the nascent stages of the fetal brain development,” said Yojet Sharma, PhD scholar and lead author of the latest paper published in the journal EMBO Molecular Medicine.
No developing brain disorder can be undone. Moreover, the degrees of intellectual disabilities are subject to vary from person to person. An intervention to treat this disorder can be planned only when its root cause in a developing fetal brain is identified.
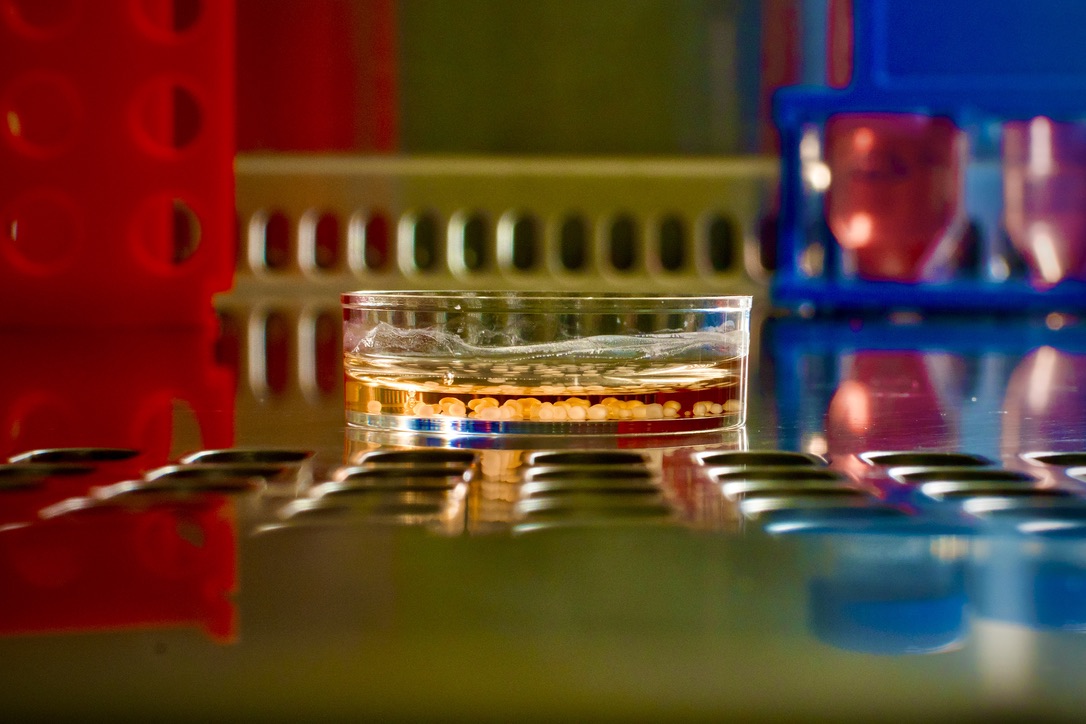
With practically no access into the developing fetal brain, researchers at the Rohini Nilekani Centre for Brain and Mind (CBM) at NCBS resorted to using stem cell technology. Professor Raghu Padinjat’s lab at NCBS generated human induced pluripotent cells (IPSC) in-house from three patients diagnosed with LS. From iPSCs, the team generated brain organoids, nicknamed mini brains, in the laboratory.
“This feature of the brain organoids makes it extremely useful to get a sneak peek to the developing human brain”, said Sharma.
Brain disorders can be a combination or a result of either genetic, environmental or nutritional factors, shared Padinjat, Senior Professor at NCBS.
“Ours is an example of how stem cell-based laboratory models allow researchers and clinicians to recapitulate the brain development process in a lab, particularly in many of these understudied and rare conditions, like LS,” said Padinjat, who is one of the co-authors of the paper.This model, the CBM team said, could help design treatments and personalised therapeutics for those diagnosed with LS. This is for the first time in India that a model system has been proposed for LS treatments and it has shown potential to be used in designing treatment regimes for such patients.
One of the hurdles of studying LS and many other rare diseases is the lack of animal models that replicate human disease, remarked Professor Alok Bhattacharya, Professor of Biology at Ashoka University.
Of the many thousands of enzymes present in the human body, an enzyme called OCRL helps maintain a balance between phospholipids. These are tiny molecules that build and maintain the health of cell membranes. Electrical pulses fired by neurons pass through these cell membranes making phospholipids vital for brain functioning. Functionally, OCRL initiates chemical reactions that help break down these phospholipids, which, in this case, are identified as PI(4,5)P2.
A missing OCRL enzyme leads to an imbalance between the phospholipid levels which, in turn, severely affect the brain's cellular functioning. Any mutation in OCRL leads to the development of LS.
“But when the concentration of PI(4,5)P2 goes anomalously high, as in case of LS patients, it silences the normal neuronal communication in the brain. We observed this phenomenon in brain organoids after one month into the experiment. The population of astrocytes (another cell type found in the brain) was abnormally high,” Sharma shared.
Now that the cause leading to the brain disorder was known, the CBM team tried to test a drug for its efficacy with an objective for designing a therapy for LS patients.
They introduced a repurposed drug to the lab-generated brain organoids and nerve cells.
“Within seven days of inducing with a repurposed drug, we observed that the PI(4,5)P2 levels dropped. The neuronal cell communication was restored to normalcy,” said Sharma.
“This study demonstrates the power of a well-designed study and modern tools in identifying molecular defects associated with a rare disease. Lowe syndrome (LS) is an ultra-rare disease affecting only a minuscule number of individuals. This study is a clear example of the power of cellular models and mechanistic exploration in identifying drugs for rare diseases,” said Prof. Bhattacharya









0 Comments