Parkinson’s Disease (PD) is no longer seen solely as a brain disorder affecting movement. It is a multi-system disorder that causes a gradual decline in multiple cellular processes throughout different cells and tissues of the body, in the early stages. Current research is investigating the causes of cellular dysfunctions that occur during the early stages of the disease, long before the classic symptoms of neuronal degeneration become apparent.
A recent study from Prof. Gaiti Hasan’s lab at NCBS looked at early-stage Parkinson’s disease caused by a mutation in the PLA2G6 gene, which is known to be associated with neurodegeneration.
The PLA2G6 gene codes for an enzyme that helps maintain healthy cell membranes. One of its key functions is to break down specific phospholipids, releasing free fatty acids and other lipid molecules that are important for various cellular processes.
“Mutations in the PLA2G6 gene are linked to compromised catalytic activity, leading to multiple genetic and neurodegenerative disorders in kids. In PLA2G6-associated Parkinsonism, the catalytic activity is intact. It is also linked to calcium metabolism in the cell and mitochondrial dysregulation,” says Thasneem Musthafa, the lead author of the study.
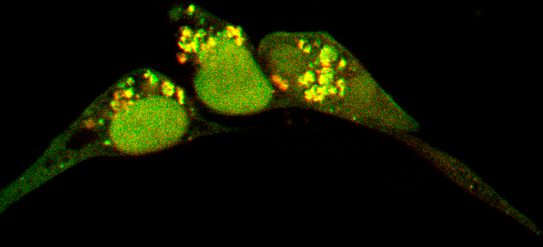
The study examined mitochondrial function and related cellular mechanisms affected by this mutation in induced Pluripotent Stem Cells (iPSCs) derived from PD patients. This is the first to investigate PLA2G6-associated Parkinson’s Disease in cell types beyond brain cells.
“PD patient-derived iPSCs offer a unique opportunity to study Parkinson's in a dish, sidestepping the ethical concerns associated with human embryonic stem cells (ESCs). Specifically, iPSCs carrying a Parkinson's disease-associated mutation allow us to explore the underlying mechanisms of the disease”, says Dr Renjitha Gopurappilly, corresponding author of the study.
Impaired mitochondrial function is one of the key hallmarks of Parkinson’s disease. Mitochondria produce energy in the form of ATP in the cells. When mitochondria malfunction, energy shortages can lead to loss of neuronal cells. Researchers measured the ATP production from iPSCs derived from PD patients with the PLA2G6 mutation and found that they produced less ATP than the cells without the mutation.
But mitochondria are not the only way cells can produce energy. When mitochondrial ATP production fails, cells ramp up ATP generation through glycolysis– the breakdown of glucose molecules. They observed that in PD patient-derived iPSC lines, this compensatory glycolytic activity was high.
Mitochondrial dysfunction does not occur in isolation. It also disrupts other interconnected cellular processes. These include calcium metabolism, mitochondrial membrane potential, and autophagy, the cellular cleanup system facilitating the removal of dead cells and debris. The research group also noted disruptions in these pathways in the PD-derived iPSCs.
“We found that these changes are evident even in non-differentiated state (early-stage) iPSCs”, says Musthafa, revealing that the same cellular pathways affected in neurons were also affected in non-neural cell types.
With Parkinson’s disease now being increasingly recognised as a multisystem disorder, understanding the associated early cellular changes could help identify biomarkers for early diagnosis. Patient-derived iPSCs could offer a powerful in vitro model to study and characterise these early cellular and developmental changes.
“Animal models, despite their necessity for studying complex brain networks and evaluating therapeutic approaches, have only partially replicated the pathology of PD. The onset, progression, and disease outcomes in these models are incomplete when compared to clinical characteristics observed in patients”, says Gopurappilly. “In contrast, in vitro iPSC-derived models provide a controlled environment to investigate specific pathogenic mechanisms and the roles of genes and proteins involved”.
“The cellular basis of late-onset Parkinson's Disease (PD) has been modeled extensively in Drosophila and C. elegans, where studies implicate loss of Ca2+ signaling and mitochondrial function as an early phenotype. Does this happen in human PD conditions? In this paper, we tested whether iPSCs derived from an early-onset PD patient show impaired Ca2+ signaling and mitochondrial function. Our results support the idea that early-onset PD mutations could have effects across multiple organs and underline the importance of studying PD across a range of model systems”, says Professor Gaiti Hasan, senior author of the study.









0 Comments